Allogeneic Mesenchymal Stem Cells: a step into the future for patients with degenerative osteoarthritis
Marianne Lomberg BVSc Hons

With improvements in health care and nutrition, our companion animals are living longer. Unfortunately, that also means degenerative conditions such as osteoarthritis are being diagnosed at an increasing rate in dogs, cats and horses.
When inflammation goes bad: the molecular basis of degenerative osteoarthritis
Degenerative joint disease is a physiological condition as much as a mechanical one. Macroscopically, it is the wearing away of intra-articular cartilage at a rate higher than the body’s ability to repair it. Physiologically, though, the process is more complex.
The breakdown of cells causes the release of pro-inflammatory cytokines and other catabolic mediators in the joint. The purpose: to attract cells which can clean up the damaged tissue, revascularise and build new tissue to replace it. In a discrete, acute injury, this works perfectly.
However, in animals with chronically unstable joints, the ongoing damage occurs faster than the body can repair it. The result is an ongoing inflammatory cytokine response which causes a continuous catabolic state and with it, chronic pain. (Sutton et al, 2009)
Rebalancing the inflammatory response
Interventions for degenerative osteoarthritis are aimed at either reducing the speed of breakdown or increasing the speed of regeneration, to the point where balance is restored. This can be done in four ways:
1) Reducing the inflammatory response through medication or dietary anti-inflammatory supplementation slows the catabolic process. However, in highly catabolic states or very unstable, far-progressed joints, these alone are insufficient to ensure the return to quality of life for patients.
2) Reducing mechanical pressure on the affected joints through surgery, weight management or exercises aimed at strengthening the surrounding muscles. This reduces the cause of joint wear, but it doesn’t correct the molecular process and therefore may not be sufficient for returning quality of life.
3) Placing an inert barrier between the nerve-containing tissues in affected joints. Intra-articular installations of viscoprosthetic agents such as polyacrylamide (Noltrex™, distributed in SA by V-Tech), provide this mechanical pain relief and can be life-saving in patients where owner finances or patient age do not allow corrective interventions, but the fact that a viscous, infiltrative foreign body is being permanently placed in a joint reduces its desirability in younger animals.
4) Encouraging tissue repair. In the past, this was achieved by placing the building blocks of the damaged cells into the body and relying on existing cells to use them appropriately – think dietary glucosamine supplementation or hyaluronic acid injections – or by focusing the body’s repair response on the damaged tissue – the principle used in Platelet Rich Plasma treatments. Recently, veterinarians have been able to add stem cell therapy to the regenerative modalities used.
What makes stem cells different from other regenerative modalities?
In fact, every treatment modality aimed at increasing the rate of tissue repair relies on stem cells.
In Platelet Rich Plasma (PRP) administration, the aim is to degranulate platelets before administration. This causes the release of chemotactic agents which attract leukocytes (to clear up the damaged tissue fragments) and haematopoietic progenitor cells – stem cells primed to become blood vessels. So PRP is essentially a way of directing the body’s stem cells towards treated areas.
Autologous Stromal Vascular Fraction (SVF) administration, goes one step further. When using this method, practitioners harvest mesenchymal fat. The fat is prepared with the aim of isolating and concentrating the stem cells. SVF administration delivers stem cells directly to the area where they’re needed. However, preparation is costly and time-consuming, and it is impossible to verify how many viable stem cells are being administered.
This is why Allogeneic Mesenchymal Stem Cells have become the most desirable tool for enhancing the physiological process of tissue regeneration. After harvesting visceral fat, the cells are not simply isolated and concentrated as with SVF, but then cultured (encouraged to multiply). In the process, Major Histocompatibility Complex (MHC) type II surface markers which identify cells as originating from a different host animal, are also removed. This means that stem cells from one donor can be used in a different patient – making allogeneic mesenchymal stem cells (MSCs) an off-the-shelf solution.
The benefits of allogeneic MSCs over autologous Stromal Vascular Fraction
- Reliable quantities of stem cells in every ml
- Guarantee that the cells being administered are viable stem cells: flow cytometry carried out on every batch tests for the absence of leukocytes and the presence of the markers of viable stem cells.
- Absence of MHC markers that would identify cells as originating from a different host
- Ease of preparation since the cells arrive ready for administration.
- Significantly lower cost than for SVF – less than half the cost in most markets and most animals. While PRP treatment needs to be administered every 6 months to retain its effect, a single administration of allogeneic stem cells has been shown to have a duration of effect of significantly over 2 years – up to 5 years in some studies, yet the cost is generally lower than a year of treatment with PRP (Alves 2021, Kriston-Pál 2020)
Taking the step into the future: what to know before applying allogeneic MSCs for the first time
Allogeneic MSCs are contraindicated in patients with active infections, and not recommended for patients with a history of neoplasia, but may become a valuable new tool to enhance quality of life for our patients.
References
Sutton S, Clutterbuck A, Harris P, Gent T, Freeman S, Foster N, et al. The contribution of the synovium, synovial derived inflammatory cytokines and neuropeptides to the pathogenesis of osteoarthritis Vet J. 2009;179(1):10–24.
Alves, J.C., Santos, A. & Jorge, P. Platelet-rich plasma therapy in dogs with bilateral hip osteoarthritis. BMC Vet Res 17, 207 (2021). https://doi.org/10.1186/s12917-021-02913-x
Kriston-Pál É, Haracska L, Cooper P, Kiss-Tóth E, Szukacsov V, Monostori É. A Regenerative Approach to Canine Osteoarthritis Using Allogeneic, Adipose-Derived Mesenchymal Stem Cells. Safety Results of a Long- Term Follow-Up. Front Vet Sci. 2020 Aug 13;7:510. doi: 10.3389/ fvets.2020.00510. PMID: 32903517; PMCID: PMC7438407.
Conflict of interest statement:
The author is a shareholder in a company that manufactures allogeneic MSCs for veterinary use.
This article was sponsored by V-Tech, the agent that supplies VetRenew stem cells (www.vetrenew.co.za) in Southern Africa. For more information or product support contact your local V-Tech representative or Customer
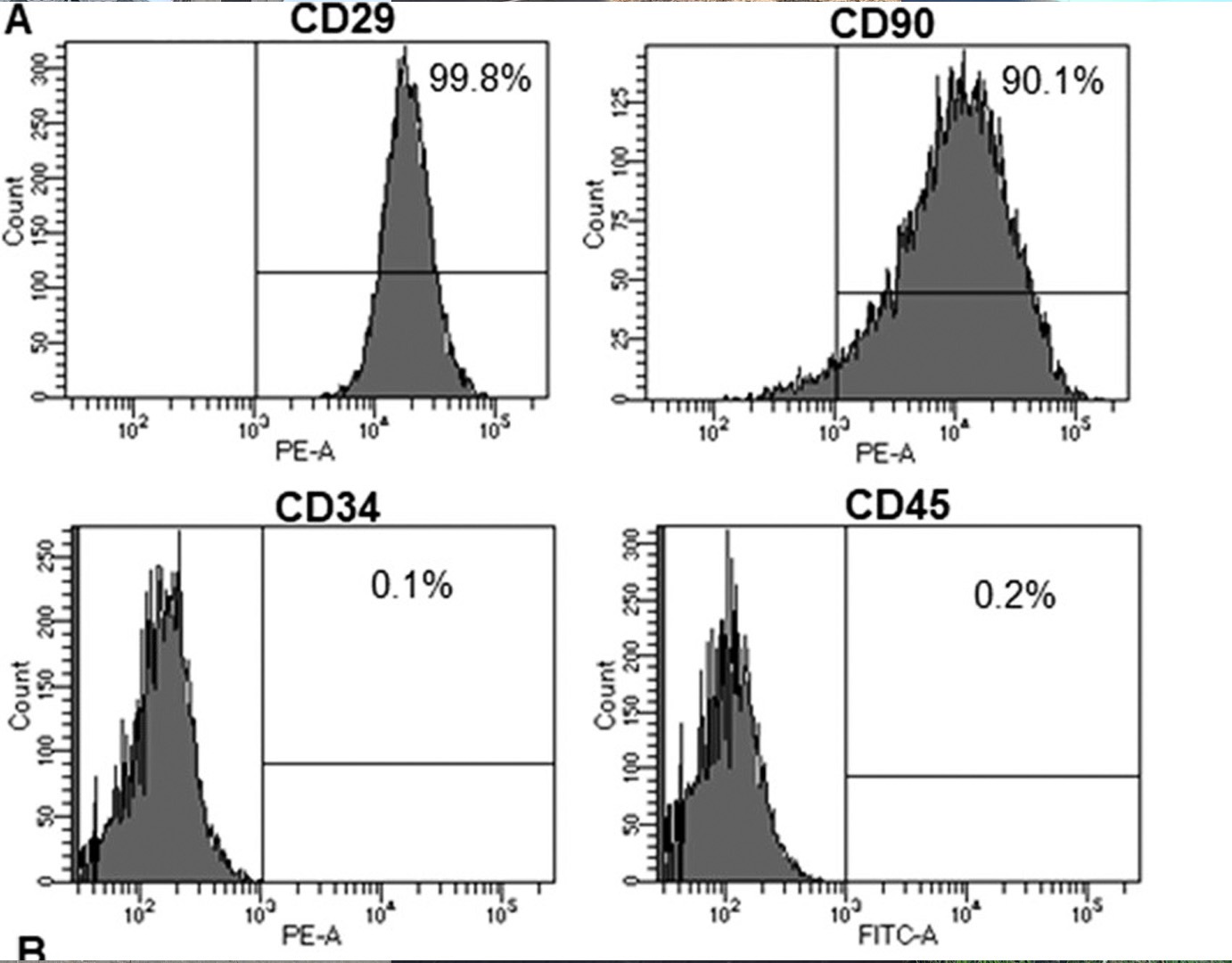
Figure 1: an example of a flow cytometry batch analysis on allogeneic stem cells. CD29 and CD90 surface markers indicate the presence of viable stem cells, absence of CD34 and CD45 markers indicates the absence of angiogenitor- and white blood cells.